Olivia Paulik, St George Hospital
About
St George Hospital is the largest hospital within South Eastern Sydney Local Health District, located in Kogarah about 15km from the Sydney CBD. It is well known for being one of NSW's major centres for trauma, and specialities include cancer services, critical care, cardiothoracic surgery, mental health services and women's and children's health care.
A multidisciplinary team from the Aged Care Precinct worked on falls prevention as part of the CEC's Leading Better Value Care Falls in Hospital Collaborative, focusing on medication review. The team consisted of Olivia Paulik, Robyn Whitaker, Kristine Tobin, Carissa Saunderson, Charlotte Bryant, Nimmy Anice Mani and Dr Yun Xu, with CEC team members Lolita Java and Paul Hudson providing coaching and support.
What they achieved
The team undertook a baseline audit of falls prevention practices to help them better understand what changes they could make to reduce and prevent falls. Psychotropic medications are commonly prescribed for elderly patients being treated in acute care, often newly prescribed following episodes of patient agitation or aggression which are not always clinically indicated. Inappropriate use of psychotropic medications in elderly patients may unnecessarily increase the risk of falls and harm.
The team set two aims for their improvement work:
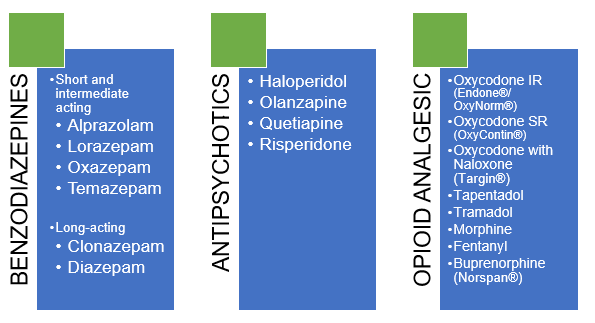
- In six months, 50% of all patients admitted to the aged care precinct under a geriatrician will be screened for target medications (antipsychotics, benzodiazepines and opioids) within 24 hours
- In 12 months, 50% of all patients who experience an episode of agitation or aggression within the aged care precinct will have a multidisciplinary safety huddle completed within 24 hours.
The team used flow charts (or process maps) to help them better design processes for medication review and post-agitation safety huddles. Using Plan-Do-Study-Act (PDSA) cycles, the team trialled a series of changes, which included:
- Introducing lanyard cards to help medical and nursing staff identify medicines that are associated with a high risk of falls
- Prompting review of medicines associated with a high risk of falls with a sticker placed in the patient’s medical notes
- Commencing safety huddles after a patient has experienced an episode of agitation or aggression.
Some medications that may cause/contribute to falls
Numerous factors are associated with an increased risk of falling and fall-related injuries among older adults, but none are as potentially preventable or reversible as medication use.1,2,3
Figure 1: Content of lanyard card to raise awareness of medications that may increase falls risk
The safety huddles helped the team identify two common issues – pain and constipation – in patients that experienced agitation. A series of PDSAs that prompted non-verbal pain assessment methods for patients that have cognitive impairment were then introduced.
The team used process measures for medication review to determine whether their changes were having an effect and whether the effect was sustained over time. Some interventions required further tailoring to help the team achieve their aim. The team were proud to share that by the conclusion of the Falls in Hospital Collaborative, there had been 269 days without a fall resulting in serious harm in the Aged Care Precinct.
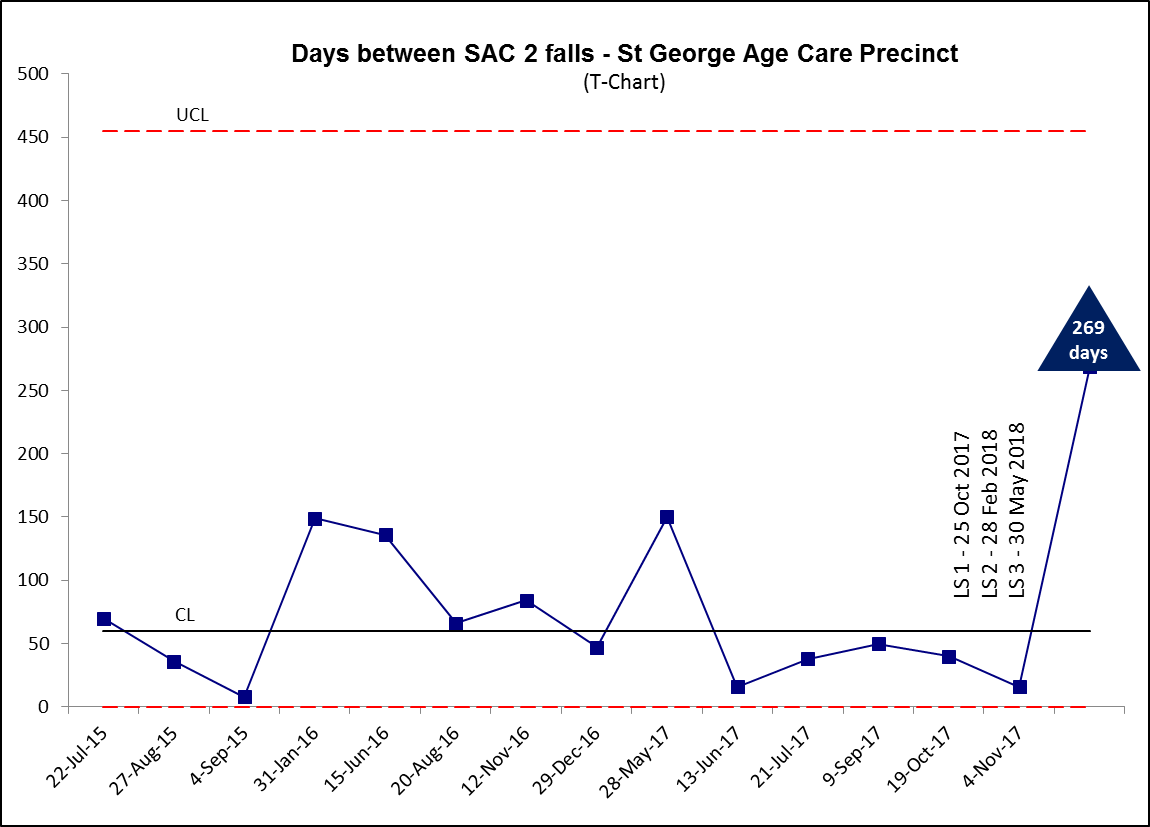
Figure 2: Days between SAC 2 Falls - St George Aged Care Precinct

We spoke to Olivia Paulik, Team Leader, at the conclusion of the Falls in Hospital Collaborative about her experience and what she learned.
What are the three things that have had the greatest impact on this quality improvement work?
The three things that had the greatest impact on our progress throughout this quality improvement work were: the framework provided by the CEC which gave our team a shared understanding of the principles and how to apply them to our clinical practice; the support that we had from our coaches - both in our regular coaching calls as well as at the learning sets; and the engagement of our multidisciplinary team in the Collaborative.
What do you think were your greatest barriers for this quality improvement work?
Our team had previously been involved in a number of quality improvement programs and we were feeling fatigued by those projects. We were initially reluctant to participate in the Collaborative as we were unclear how this process was going to different to the previous programs we had been involved with. However once we attended the first learning set we had a much clearer understanding of what the Collaborative could offer us, and we became inspired to participate. Once we commenced the Collaborative, the team became very engaged in the process, and the improvements we achieved were beneficial to both our team as well as our patient’s outcomes.
What effect has your involvement in this collaborative had on your patients?
We have now gone over 300 days without having a serious fall incident. In the 12 months prior to commencing the Collaborative, we had six serious (SAC 2) fall incidents in aged care. Although our overall falls rate has not changed markedly during our participation in the Collaborative, we made a really significant impact on the rate of serious injury in our patients.
Have you had good engagement with other team members from a multidisciplinary perspective?
Yes, we've had very good engagement from a multidisciplinary perspective in our Collaborative. We have got a number of multidisciplinary specialties that are represented in our team and are very engaged in the process. I think that the success of our improvement initiatives is due to the strength of the relationship between our multidisciplinary team members.
Do you think you can apply the QI methodology that you've learnt to other areas? How so?
We can definitely apply the QI methodology that we have learned into other areas. I think that we are really only in the very beginning stages of a lot of our improvement work. The tools, frameworks and processes that we have learned throughout this Collaborative will definitely be useful as we continue to progress this project as well as start new quality improvement initiatives.