Biannual Incident Report
July 2023 – June 2024
Incident Management in NSW Health
An incident is an unplanned event that results in, or has the potential for, injury, damage or loss, including near misses. An incident may also be referred to as an ‘adverse event’. 1
NSW Health is committed to learning from incidents and requires all staff to report patient-related (also referred to as clinical), worker and visitor incidents, near misses, and consumer feedback. This reporting ensures that risks to patient safety are recognised and action taken to reduce the risk of them happening again. This commitment to patient safety is supported by the NSW Health Incident Management Policy Directive PD2020_047.
NSW Health has reported on incidents since 2005, when the Incident Information Management System (IIMS) was introduced. From October 2019 to December 2020, a new system, ims+, was progressively introduced across NSW Health. St Vincent's Health Network (SVHN) use an alternate product, Riskman, for their incident reporting.
Patient-related incidents reported in ims+ are assigned a Harm Score, which is applied based on the severity of the outcome for the patient and any additional care required due to the incident. The Harm Score directs the level of investigation and action required, with four Harm Score ratings ranging from Harm Score 1 (serious harm) to Harm Score 4 (no harm or near miss).
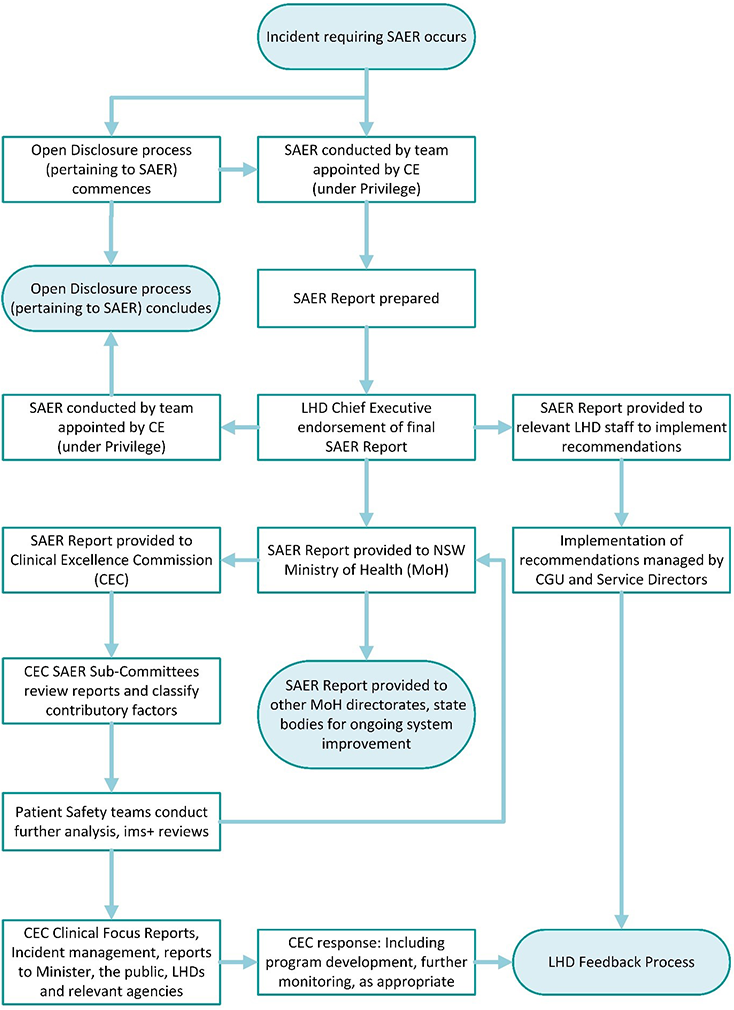
In line with the NSW Health Incident Management Policy, clinical Harm Score 1 incidents must undergo a Serious Adverse Event Review (SAER). Approved SAER investigation methodologies aim to identify factors that caused or contributed to an incident including any systems issues. Recommendations are made by SAER teams to reduce identified risks. Actions taken are tracked by relevant Local Health Districts (LHDs) or Specialty Health Networks (SHNs). Lessons are shared with the broader health system as necessary.
Clinicians undertake a structured process to review incidents, focusing on understanding what happened, how and why it happened and what could be done in future to reduce risks. Figure 1 provides the framework for the review process for incidents requiring a SAER during the July 2023 – June 2024 reporting period.
The NSW Ministry of Health (MoH) is notified of Harm Score1 incidents, including Australian Sentinel Events (ASE), and other significant clinical incidents through a Reportable Incident Brief (RIB).
Sentinel Events are rare incidents that are considered to be wholly preventable and result in serious harm or death to a patient. Since 1 July 2019, ten ASE types have been nationally determined and reported. Further information on Sentinel Events can be obtained from the Australian Commission on Safety and Quality in Health Care website.
Figure 1: Serious clinical incidents requiring SAER investigation during the period July 2023 – June 2024.
The CEC's role in Incident Reporting
The Clinical Excellence Commission (CEC) is the lead agency supporting patient safety and clinical quality improvement in the NSW public health system. The CEC plays a key role in monitoring clinical incidents reported in NSW and analysing incident data to determine priority areas for improvement.
The CEC supports patient safety across NSW through programs and expertise including:
- Recognition and management of the deteriorating patient,
- Sepsis management,
- Comprehensive care Minimising Harm model,
- REACH (Recognise, Engage, Act, Call, Help is on its way) and
- Infection Prevention and Control (IPAC).
NSW Health was the first Australian jurisdiction to publicly report healthcare incident data in 2005. The CEC published its first online clinical incident management report in 2013. Regular publication of this report reflects the CEC's commitment to be transparent, accountable and supportive of NSW Health clinicians and staff to provide the safest and highest quality care for every patient, every time.
In this report
This report includes data from multiple sources including ims+, RIBs, SAERs, Riskman, the Health Information Exchange (HIE) and Enterprise Data Warehouse (EDWARD).
This report contains an analysis of patient-related incidents and consumer feedback reported in the NSW Health incident management system ‘ims+’ and St Vincent’s Hospital Network incident management system ‘Riskman’ between July 2023 – June 2024. It builds on previous reports and will continue to evolve and enable comparison between reporting periods and the identification of trends.
Due to changes in reporting, including Australian Sentinel Events and NSW Health’s transition to ims+, data in this report cannot be compared to data from reports prior to 2021.
This report contains:
- An explanation of how to interpret the data
- Patient-related incident data
- Patient-related RIB data
- Systems and risks factors in serious clinical incidents identified through SAER investigations
- Sentinel events
- Consumer feedback including complaints and compliments.
Data considerations
Analysis of the information contained within ims+ can provide insight into how incidents occur, relevant clinical context, highlights issues and identifies system-related opportunities for improvement. However, due to wide variation between services and facilities, it is difficult to make accurate comparisons based on notification numbers alone. Many factors influence incident reporting. Incident reporting counts or rates should not be used as the sole source of benchmarking data for any project, program, facility or health organisation.
Importantly, lower rates of reporting are not a reliable indicator of safer care. A qualitative rather than quantitative interpretation of the data is recommended. These data do not constitute an epidemiologic data set, and conclusions should not be drawn about the relative frequency of events or trends in events over time.
Incident data are considered a ‘live’ dataset, variation in reported numbers is expected as health services update incident information and consumer feedback reports. The CEC has taken great care to ensure the information provided within this report are accurate and up to date at the time of data extraction. Data for all reporting periods contained within this publication will be refreshed and updated with each future release. As such, the information and figures provided in published reports may change without notice.
References
1Organisation for Economic Co-operation (OECD) (2017).
