Patient-related incident data
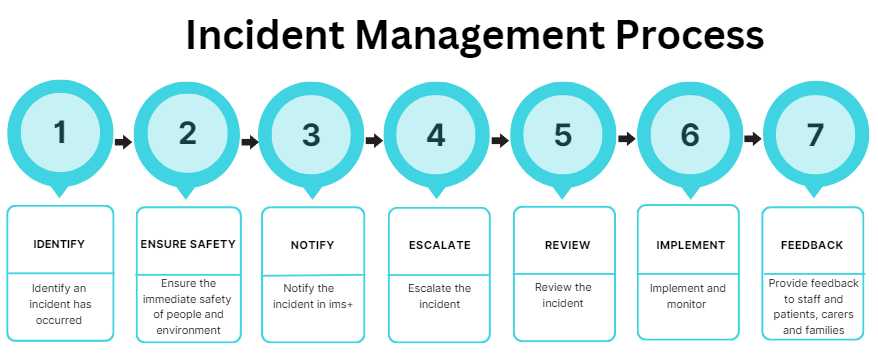
Incident Management Process
NSW Health is committed to learning from incidents. When an incident occurs, the health service follows a series of steps to understand and address underlying system issues. The steps are displayed below.
Figure 2.
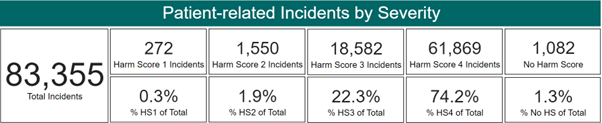
Severity of patient-related incidents
Patient-related incidents notified in ims+ and Riskman are allocated a Harm Score, which directs the level of review and action required for an adverse event. The Harm Score is based on the severity of the outcome for the patient and any additional care or treatment needed following the incident. The Harm Score is automatically calculated in ims+ based on staff selections.
A manager confirms the Harm Score as soon as possible after the incident is notified. The most serious incidents are rated as a Harm Score 1. The other possible scores, in descending order of severity, are Harm Score 2, Harm Score 3 and Harm Score 4.
Incident notification volumes by reporting period are depicted in Figure 3. During the most recent 6 month reporting period, January 2024 to June 2024, a total of 89,331 patient-related incident notifications were reported by NSW Health public hospitals and St Vincent’s Health Network.
The majority of these incidents (96% per cent) were rated as a Harm Score 3 or Harm Score 4 which resulted in minor or no harm to the patient. Serious patient-related incidents in health care are extremely rare, with 2.2 per cent of incidents notified rated as Harm Score 1 or Harm Score 2.
Incidents without a confirmed Harm Score are generally indicative of an investigative timeframe delay, from the initial notification of an incident to the review and confirmation by a manager. At the time of publication, unassigned Harm Scores accounted for 2 per cent of all reported patient-related incidents during the January 2024 – June 2024 6 month reporting period. Breakdown by Harm Score is displayed at Figure 4.
Figure 3.
![]()
*All data obtained from ims+ and Riskman. Excludes data relating to private hospitals.
Figure 4.
*All data obtained from ims+ and Riskman. Excludes data relating to private hospitals.
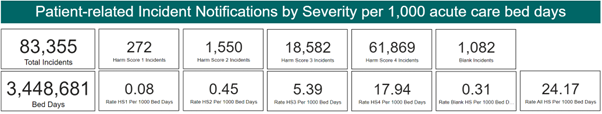
Measuring patient-related incidents
Reporting the number of patient-related incidents in relation to hospital activity provides greater insight and context than reporting on the actual number of incidents alone. NSW Health uses a rate-based calculation of incidents recorded per 10,000 inpatient separations (all inpatient episodes of care in public hospitals across NSW). This measure allows NSW Health to compare the rate of incidents by their severity over time, according to activity. The rate does not account for patient complexity.
The rate of patient-related incidents per 10,000 separations has remained steady over time. Figure 5 below provides an overview of rates by Harm Score and reporting period.
Figure 5.

*All data obtained from ims+ and Riskman. Excludes data relating to private hospitals.
During the most recent reporting period January 2024 – June 2024, the patient-related incident rate was 907 per 10,000 inpatient separations*.
Figure 6.

*All data obtained from ims+ and Riskman. Excludes data relating to private hospitals.
Separation data from July 2021 onwards was extracted from the Enterprise Data Warehouse (EDWARD). Data prior to this period have been extracted from the Health Information Exchange (HIE).
Principal Incident Types
When a patient-related incident is notified, staff select one of the 25 Principal Incident Types (PITs) available in ims+ to describe the incident in further detail.
During the review process, managers review and confirm the selected PIT. Some PITs are divided into sub-categories, known as Level 2 and Level 3 PITs, allowing these incidents to be further categorised. The top five PITs by volume for the January 2024 – June 2024 reporting period are displayed below. These align with previous reporting periods.
Figure 7.

*Data includes patient-related incidents (all Harm Scores) recorded within ims+ during the reporting period.
Excludes data relating to private hospitals and St Vincent’s Health Network.
Concerning Behaviour
Incidents related to a patient’s behaviour are classified using the Concerning Behaviour PIT. This category includes physical and/or verbal aggression, self-harm, risk taking and patients absconding from care.
Across the January 2024 – June 2024 6 month reporting period, 98 per cent of concerning behaviour incidents were assigned as either a Harm Score 3 or Harm Score 4.
Patient related aggression including verbal and/or physical aggression accounted for over half of all reported Concerning Behaviour incidents. The most frequently selected sub-categories relating to Concerning Behaviour were:
- Aggression – both physical and verbal (29 per cent)
- Aggression – physical (17 per cent)
- Aggression – verbal (12 per cent)
- Non-adherence (8 per cent).
Falls
Patient falls in hospital can be a major cause of harm and may result in increased hospital length of stay. Hospitalised patients older than 65 years of age have a significantly higher risk of falling.
The prevention of falls is a significant health issue, and minimising harm by focusing on key factors such as frailty, cognitive impairment (dementia and delirium), poor mobility, medications and nutrition can assist in reducing poor outcomes for older people.
Incidents relating to patient falls, slips, trips or near misses are notified under the Falls PIT in ims+. During the January 2024 – June 2024 6 month reporting period, 96 per cent of all falls related incidents recorded within ims+ resulted in minimal to no harm to the patient (Harm Score 3 or Harm Score 4).
The CEC Comprehensive Care – Minimising Harm safety model aligns with the National Safety and Quality Health Service Standards (NSQHSS), Comprehensive Care and Partnering with Consumers standards. Further information on falls prevention can be found on the CEC website.
Skin Integrity
Many factors can influence skin integrity, including a person’s age, mobility, body weight and external factors such as pressure or moisture. The Skin Integrity PIT contained within ims+ enables the notification of skin specific issues including pressure injuries, skin tears, bruises, moisture associated skin damage, lacerations and burns.
During the January 2024 – June 2024 6 month reporting period, the majority (97 per cent) of reported Skin Integrity related incidents were assigned either a Harm Score 3 or Harm Score 4, which resulted in minor or no harm to the patient. Skin Integrity related incidents mainly related to:
- Pressure injuries (59 per cent)
- Skin tears (26 per cent)
Pressure injuries (also referred to as pressure ulcers or bed sores), are injuries to the skin caused by unrelieved pressure and may occur when patients are unable to move due to illness, injury or surgery. Pressure injuries can happen from lying or sitting in the same position for too long. They can be painful and may take a long time to heal.
Skin tears are injuries to the skin that may be caused by falling or bumping into furniture. Skin tears occur mainly in the elderly as skin can be more fragile and prone to damage more easily. Some medications, such as steroids can make the skin thinner. Further information relating to pressure injuries and their prevention can be found on the CEC website.
Medications/IV Fluids
Use of medicines is one of the most common therapeutic interventions in Australian hospitals. It is also among the most complex, with the delivery of each dose of medicine involving up to 30 steps and nearly as many individuals.
Documenting specific details of medication related incidents is essential for accurate reporting and helps to identify risks and areas for improvement.
The majority of Medication/IV Fluid incidents reported in ims+ during the January 2024 – June 2024 6 month reporting period (96 per cent) were allocated a Harm Score 3 or Harm Score 4, resulting in minor or no harm to patients. 78 per cent of all medication/IV fluid incidents notified related to the administration and prescribing of medications.
Administration related incidents include medications being administered incorrectly, for example an oral medication administered instead of intravenous, the wrong amount given, or medications given at the wrong time. Prescribing related incidents include where the wrong medication or wrong dose are prescribed. Incidents may also include where a medication was omitted or not prescribed or where
the medication was prescribed with a known contraindication.
The CEC’s Medication Safety team supports the safe and quality use of medicines by identifying and addressing emerging medication safety risks as well as monitoring, evaluating and optimising medicines use across NSW. Further information on medication safety can be found on the CEC website.
Treatment and General Care
The Treatment and General Care PIT is used to identify issues specifically relating to the treatment or care of a patient, and includes treatment that is declined, delayed or inadequate and incorporates accidental injury caused to the patient during medical care.
During the January 2024 – June 2024 6 month reporting period, 93 per cent of Treatment and General Care related incidents were confirmed as a Harm Score 3 or Harm Score 4. Of all Treatment and General Care incidents reported, the majority were categorised as involving:
- Inadequate treatment or care (32 per cent)
- Delayed treatment or care (28 per cent)
- Omitted treatment or care (10 per cent)
Reportable Incident Briefs (RIBs)
In line with the NSW Health Incident Management Policy, confirmed Harm Score 1 incidents are submitted to the NSW Ministry of Health as a Reportable Incident Brief (RIB) within 24 hours of being notified. Other Harm Score incidents may also be submitted as a RIB, as determined by the Chief Executive of the health service or as required under the policy.
Overall RIB notifications (all Harm Scores) have declined since mid-July 2022. This decrease may be attributed to the reduction of COVID-related RIB submissions. Figure 8 illustrates RIB volumes by severity and reporting period.
Figure 8.

*RIB data obtained from the CEC Patient Safety Database. Includes RIBs received from NSW public and private hospitals and St Vincent’s Health Network.
During the most recent reporting period, January 2024 – June 2024, the NSW Ministry of Health received a total of 359 clinical RIBs (all Harm Scores). RIBs were received from NSW public and private hospitals, as well as St Vincent’s Health Network. The majority of these RIBs (79 per cent) were confirmed as a Harm Score 1.
Figure 9.

*RIB data obtained from the CEC Patient Safety Database. Includes RIBs received from NSW public and private hospitals and St Vincent’s Health Network.
Harm Score 1 RIBs and SAERs
A Serious Adverse Event Review (SAER) must be undertaken for each Harm Score 1 RIB received, using one of the four approved review methodologies. Local health organisation Chief Executives may also direct a review be undertaken for other clinical Harm Score 2 – 4 incidents. Further details on the review methodologies can be accessed here.
The purpose of a SAER is to identify any factors that caused or contributed to the incident. Public hospitals are required to submit review findings and recommendations reports to the Ministry of Health within 60 calendar days of the incident notification. Private hospitals are required to submit SAER reports within 100 calendar days.
The CEC allocates each SAER report received to a Serious Incident Review (SIR) sub-committee, where they are reviewed and classified by subject matter experts to identify themes, system wide learning and risks. Six SIR sub-committees were operational within NSW Health during the reporting period. These sub-committees are shown below.
Figure 10.

An overview of each SIR sub-committee is provided below:
Clinical Management includes a broad category of incidents related to the diagnosis, treatment and monitoring/observations of adult patients in any inpatient, ambulatory or ambulance care setting.
Mental Health / Alcohol and Other Drugs review mental health and alcohol/drug related incidents, including concerning behaviour and the suspected suicides of mental health clients.
Maternal and Perinatal review all serious incidents related to the care of pregnant women before and after birth, as well as neonates aged between 0 to 28 days. This includes unexpected intra-partum stillbirths, perinatal and maternal deaths.
Children and Young People review health care related serious incidents involving children aged between 29 days to 16 years.
COVID-19 established in late 2021, this sub-committee review clinical cases including outbreaks and reportable COVID patient deaths. The COVID-19 sub-committee ceased operation on 31 October 2023.
Prevention and Response to Violence, Abuse and Neglect (PARVAN) this sub-committee was formed in late 2021, and focuses on cases that relate to children, young people and adults who are victims of violence, abuse and neglect. Cases are first reviewed and classified by one of the five sub-committees referred to above, before being referred to PARVAN for review and identification of themes.