Risk Assessment and Prophylaxis
The NSW Health Prevention of Venous Thromboembolism Policy (PD2024_045) requires the following patients, who are at an increased risk of developing hospital-associated VTEs, to be assessed for VTE risk:
- All adult patients (over 16 years old) admitted to hospital. This may include patients undergoing planned surgical interventions.
- Adult patients (over 16 years old) being discharged from an Emergency Department, who as a result of acute illness or injury, have significantly reduced mobility relative to their normal state, and
- All pregnant and post-partum women.
If using electronic systems, a VTE risk assessment may be recorded in the electronic medical record (eMR) or if using a state-based build Risk Assessment Tool, a completed risk assessment will automatically be recorded in the eMR.
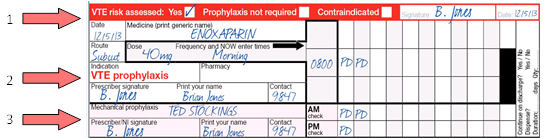
If using the standard paper National Inpatient Medication Chart (NIMC), there is a dedicated section to document that a VTE risk assessment has been completed.
Additional areas for documentation may include the patient’s health care record or locally approved forms.
For all admitted patients, VTE risk needs to be reassessed:
- Regularly (at least every 7 days)
- As clinical condition changes e.g. after surgery, changes in mobility
- At transfers of care (including discharge, with particular consideration regarding the need for extended prophylaxis).
Adult inpatients
There are many known risk factors which increase individual VTE risk and hospitalised adult patients often present with one or more of these risk factors. Common risk factors include age over 60 years, moderate to major surgery, active infection, acute medical conditions, dehydration, significantly reduced mobility normal to relative state and more.
The paper based Venous Thromboembolism VTE Risk Assessment Tool (Stock Code: NH700015) can be ordered via the Finsbury Green online ordering system.
Internationally, electronic solutions have been effective in improving VTE prevention processes and reducing rates of hospital-associated VTE.
In NSW hospitals, the state-based build electronic version of the VTE risk assessment tool is available for implementation in the Cerner eMR. Seek assistance from your local eMR application specialist/team.
To learn how to use these tools, refer to training resources in Educating Staff and Patients.
To learn how to use the eMR "VTE Risk Assessment Tool for Adult inpatients" please refer to the quick reference video. (New tool for release in 2024).
Pregnant and post-partum women
Women are at higher risk of developing VTE during pregnancy due to multiple risk factors, but the most significant reason is that clotting factor levels increase and enzymes which break down clots become less active1
Venous Thromboembolism (VTE) accounts for 9.5% of maternal deaths in Australia2. While the risk of VTE has been found to be greater during the post-partum than the antenatal period,3,4 many VTEs still occur in the first trimester4. Early risk assessment and prevention is recommended.
Evidence suggests that all pregnant and post-partum women will benefit from VTE risk assessment and prescription of appropriate prophylaxis throughout their patient journey. This includes at:
- the first antenatal review and/or booking
- hospital admission for a non-pregnancy related complaint
- hospital admission for a pregnancy-related complaint
- the time immediately after birth (post-partum).
The paper based Maternal Venous Thromboembolism VTE Risk Assessment Tool (Stock Code: NH700088) can be ordered via the Finsbury Green online ordering system.
Electronic versions of the Maternal VTE Risk Assessment Tool (Antenatal and Postpartum) were released by eHealth NSW as part of the Between the Flags (BTF) 4.1 release. They are available for implementation in the Cerner eMR. Seek assistance from your local eMR application specialist/team.
To learn how to use these tools, refer to training resources in Educating Staff and Patients.
To learn how to use the eMR "VTE Risk Assessment Tool for Antenatal and Postpartum women" please refer to the quick reference video. (New tool for release in 2024).
- Devis,P. & Knuttinen, M.G. (2017). Deep venous thrombosis in pregnancy: incidence, pathogenesis and endovascular management. Cardiovascular Diagnosis and Therapy, 7(Suppl 3), S309–S319. https://doi.org/10.21037/cdt.2017.10.08
- Humphrey MD, Bonello MR, Chughtai A, Macaldowie A, Harris K & Chambers GM 2015. Maternal deaths in Australia 2008–2012. Maternal deaths series no. 5. Cat. no. PER 70. Canberra: AIHW.
- Queensland Clinical Guidelines. Venous thromboembolism (VTE) prophylaxis in pregnancy and the puerperium. February 2014
- Royal College of Obstetricians and Gynaecologists. Reducing the risk of thrombosis and embolism during pregnancy and the puerperium. Green-top Guideline No.37a. 2009.
Patients discharged from ED
Adult patients (over 16 years old) discharged from an ED who have significantly reduced mobility relative to normal state should be assessed for VTE risk.
Patients may have a higher chance of developing a VTE if they have a lower leg injury, particularly if:
- Immobilisation is needed with a plaster cast, boot or brace.
- They cannot (or are told not to) bear weight on an injured leg or legs
- They have a severe injury such a dislocation, fracture or complete tendon rupture
These patients should undergo VTE risk assessment and be prescribed appropriate prophylaxis by an ED clinician prior to leaving the ED. All other patients to be discharged home from an ED do not need to be assessed for VTE risk.
The paper based Emergency Department (ED) VTE Risk Assessment Tool (Stock Code: NH700955) can be ordered via the Finsbury Green online ordering system or downloaded below.
This paper risk assessment tool has been endorsed for use for adult patients (> 16 years) being discharged from the Emergency Department with an isolated lower limb injury requiring temporary lower limb immobilisation.
Many NSW Health Emergency Departments have transitioned to electronic workflows and uptake of the paper tool was found to be low. For this reason, CEC has built a new electronic tool with eHealth NSW, which is currently under evaluation. In the interim, sites may use the paper tool below for risk assessments for patients or as a guide to update their current processes in the Emergency Department.
Appropriate Prophylaxis
There are two types of prophylaxis:
- Pharmacological, such as enoxaparin, heparin
- Mechanical, such as anti-embolic stockings
The choice of prophylaxis should be guided by evidence, local hospital protocol, as well as reference to drugs available on the hospital formulary. If the decision is made to prescribe pharmacological and/or mechanical prophylaxis, an order must be written in the paper or electronic medication chart.
