Diagnostic error
Diagnosis is the process of trying to understand the nature of a patient's problems to clarify their prognosis and treatment options.
Diagnostic error refers to a diagnosis that is missed, incorrect or delayed as detected by subsequent definitive information.
To further define these;
- missed diagnosis is one in which a diagnosis was never made,
- wrong diagnosis has occurred if an alternative diagnosis was made prior to the correct diagnosis being identified, and
- delayed diagnosis is one in which a correct diagnosis was made however was not determined until significant time had elapsed despite definitive information being available earlier.
Key elements
The key elements of the program focus on:
- The development of knowledge and awareness of the cognitive and system factors associated with diagnostic error
- The promotion of critical thinking at key points in the diagnostic process to identify potential risks and reduce diagnostic errors
- The provision of oversight, structure and guidance for monitoring and evaluating diagnostic processes
- Fostering partnerships with patients.
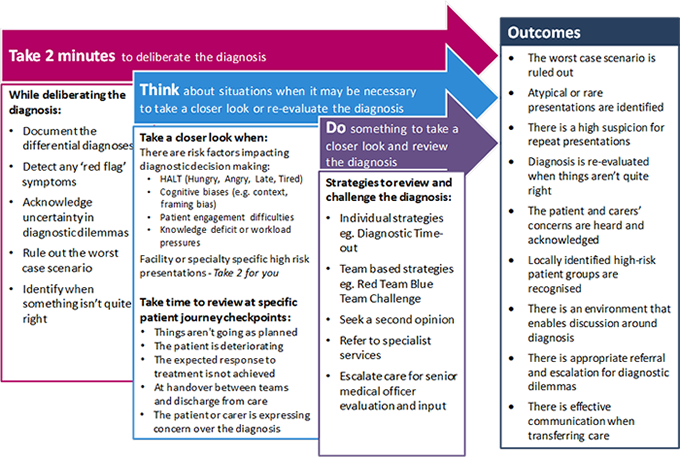
Take 2 - Think, Do is a framework to support accurate diagnostic decision-making in complex clinical environments. The framework assists clinicians to recognise when there may be a high risk for diagnostic error to occur and provides a structured process that facilitates a more detailed case review at key times in the patients' journey.
The framework consists of the following components:
- Take 2 minutes to deliberate the diagnosis - promotes a quick reflection that ensures the critical elements of diagnosis have been captured for each clinical presentation.
- Think about when to take a closer look - provides clinicians with insight into high risk clinical situations in which it may be appropriate to take a closer look or re-evaluate the diagnosis.
- Do something in these high-risk situations - provides clinicians with the strategies to take a closer look by outlining approaches that aid decision making. This includes individual and team-based strategies to critically appraise the decision-making process.
This framework promotes reflective safe diagnostic process by increasing clinician knowledge and awareness of the cognitive risks associated with decision making during diagnosis. The strategies outlined provide support, structure and guidance to decision making. This ensures all the key factors have been considered for each clinical presentation and the worst-case scenario is flagged and ruled out.
Resources for Take 2, Think, Do
View Take 2 Think Do Framework ~ 416KB
The following resources have been developed to support facilities and clinicians with the Take 2 – Think, Do framework;
The Red Team / Blue Team Challenge provides tools and a structure for clinicians to safely question and challenge the diagnostic decision-making process within a team environment. The strategy is developed and adapted from the military red team blue team exercises used for testing force readiness.
In the clinical environment, blue team members undertake history taking, clinical assessment and synthesis in the traditional manner, while red team members are tasked with questioning the decision making, identifying 'red flag' symptoms and symptoms that don't fit and then suggesting possible alternative diagnoses.
The strategy outlines:
- Guidelines for establishing the Red Team / Blue Team Challenge within clinical teams
- A series of prompts that the red team member may consider when critically analysing the clinical scenario
- Ground rules for establishing a safe environment
- Identified opportunities for challenge.
Resources for Red Team/Blue Team Challenge
The following resources have been developed to support facilities and clinicians with the Red Team / Blue Team Challenge:
- Red Team / Blue Team Challenge - Information for clinicians ~245KB
- Red Team Blue Team - Sample prompt card ~293KB
Two video resources for Red Team / Blue Team Challenge have been developed. One video provides an overview of the Red Team / Blue Team Challenge in progress highlighting the key focus points of the challenge. The other video highlights triggers for commencing a Red Team / Blue Team Challenge in the clinical environment.
Education relating to diagnostic error is aimed at increase knowledge and awareness relating to clinical decision making. The following resources have been developed to provide educational tools and support for clinicians regarding the complex issues, systems and processes impacting on diagnosis, leading to errors.
The strategies outlined provide support, structure and guidance to decision making. This ensures all the key factors have been considered for each clinical presentation and the worst case scenario is flagged and ruled out.
External resources
Jess' Story: Do no harm (11 min YouTube video)
Describes the tragic journey of a teenager who died following a diagnostic error and the cognitive and system related breakdowns that led to the missed recognition of long QT syndrome.
Onthewards: Episode 85 - Diagnostic Errors (25 min podcast) This podcast episode discusses the common causes of diagnostic error and explores the decision making process and some of the common cognitive biases in clinical practice, providing some practical strategies to help reduce error within a team.
Morbidity and Mortality reviews
Morbidity and Mortality (M&M) meetings are an ideal place to evaluate diagnostic error cases in a multidisciplinary environment that includes all the team members involved in the care of that patient.
Evaluating clinical practice and improvement
Clinical audit that compares differential diagnoses and initial diagnosis with discharge diagnosis is an ideal way to identify types and trends in diagnostic error that is not detected by other means. Looking back at these cases provides a unique insight into the accuracy of our own decision making and is an excellent teaching tool for junior clinicians.
Sample audit tools have been developed to monitor and evaluate diagnostic error practices.
- Diagnostic error: Clinical outcomes evaluation tool PDF ~116KB
- Diagnostic error: Clinical practice evaluation tool PDF ~135KB
Clinical incident management and reporting
All diagnostic errors and near misses are classified as an adverse event and as such should be reported in the Incident Management System (ims+) in the Principal Incident Type - Clinical Management, sub-category diagnosis - missed or diagnosis - delayed.
Information on clinical incident reporting and management in NSW can be found on CEC's Incident Management pages.
Patients are recognised as being important in the diagnostic process and are a part of the team. A patient or person centred approach is known to improve teamwork and communication. A focus on improving communication between clinicians and patients during history taking is an important step to aid accurate and timely diagnosis.

