COVID-19 SIR Sub-Committee
Since the COVID-19 pandemic was declared on 22 March 2020, NSW Health has provided extensive direction and support for a statewide public health response. The arrival of the Delta variant of the SARS-CoV-2 in NSW in May 2021 presented unique challenges to health and aged care facilities due to high morbidity and mortality of this variant.
The COVID-19 Serious Incident Review (SIR) sub-committee was established in late 2021, to review COVID related cases reported during July – December 2021.
This sub-committee is responsible for the review and analysis of COVID-19 SAER reports relating to outbreaks and reportable patient deaths, to identify key learnings, meeting risks and patient safety issues that have state-wide implications. Like the other SAER/SIR sub-committees of the Clinical Risk Action Group (CRAG), SAER reports referred to the COVID-19 SIR are classified according to a standardised taxonomy.
A total of 65 SAER reports were reviewed by the sub-committee during the reporting period. The main human factor elements identified within these cases related to:
- No human factors identified, following review of the SAER report
- Loss of situation awareness, relating to the fixation on irrelevant information, poor prioritisation and planning of care
- Cognitive based errors, involving the failure to understand, process or act appropriately on available information despite adequate education and knowledge.
- Skill-based – poor task execution, relating to failures in carrying out actions of a task, where the process was correct, but the execution was not
- Knowledge based errors, caused by gaps in skills or knowledge
The top 5 clinical risk factors that were considered a direct cause, or contributing factor, to the outcome of an incident related to:
- COVID-19, where the incident was directly impacted by or precautions relating to COVID-19
- Comorbidities – Physical, refers to the presence of two or more overlapping conditions in the same person
- Healthcare associated infection/multi-drug resistant organism (MRO), relates to infections acquired within in healthcare facilities
- Confusion / Delirium, where a patient experiences disturbances, attention cognition and perception that developed over a short period of time (usually hours or days)
- Acute coronary syndrome (ACS), the spectrum of acute clinical presentations resulting from underlying coronary heart disease, including heart attack and angina.
An overview of COVID-19 classifications are provided below.
Figure 17.
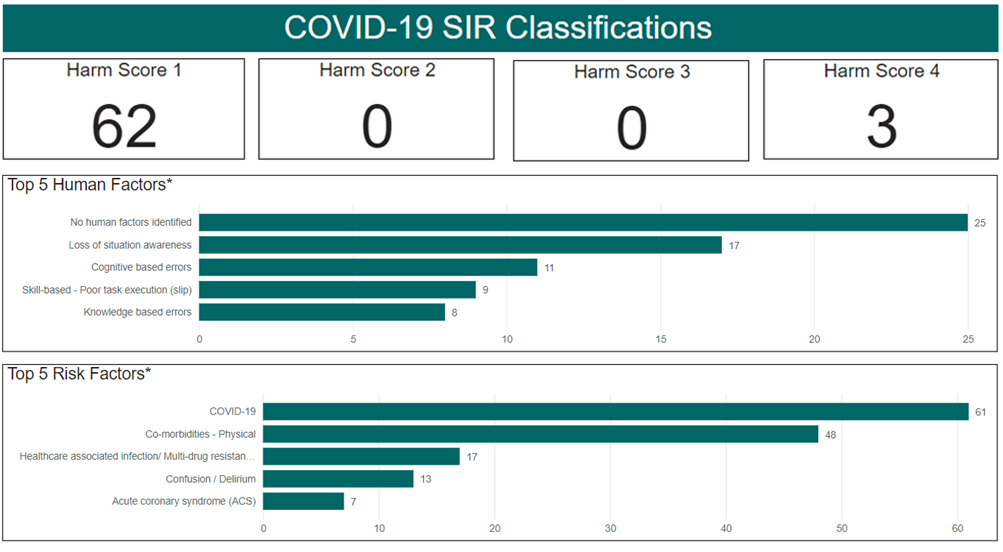
*Multiple factors can be applied to each SAER
System factors identified within the COVID-19 SAER reports predominately related to:
- Care Planning, including difficulties in organising care and high risk factors not identified or acted upon
- Communication, including inadequate information between care providers
- Environment, including physical surrounds (e.g. poor line of sight and cluttered areas).
Figure 18.
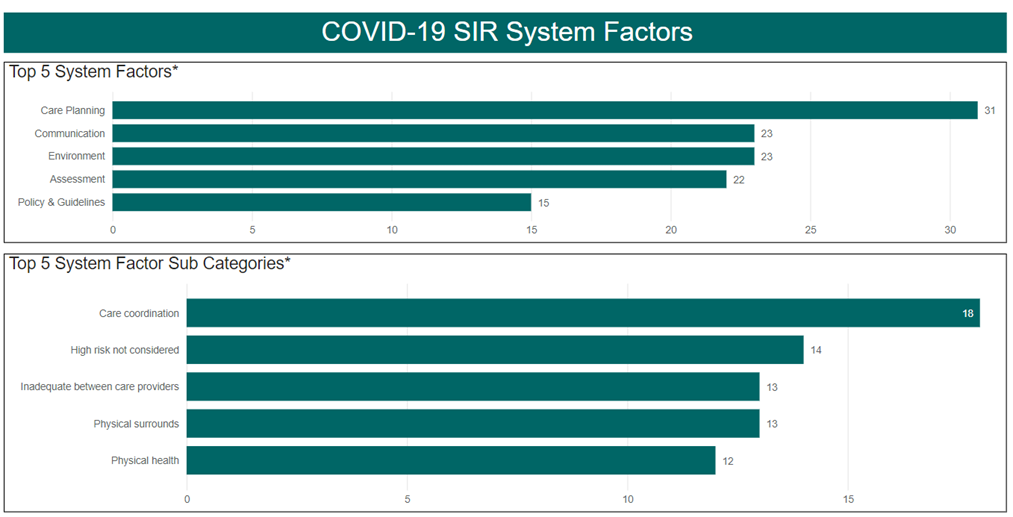
*Multiple factors can be applied to each SAER
