Getting started
This page provides guidance on building your case for improvement: identifying the problem you aim to improve (not solution), backing up with local data and gaining health service support to establish your quality improvement team.
It is important to determine a realistic timeline prior to starting the improvement project. As a guide, it can take 12 to 18 months to initiate, test, implement and sustain an improvement.
Note: This timeline may be shorter if previous improvement efforts have been made and may be longer if the change is complex and/or involves different services and departments.
What is the problem you want to solve?
Start by identifying the problem you aim to improve. You can do so by gathering local data and conducting a literature review. It is important to focus on the problem not the solution at this phase.
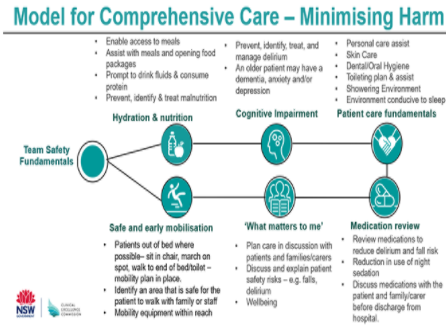
The Older Persons' Patient Safety Program has developed a safety model Comprehensive Care – Minimising Harm, which focuses on how we safely care for older people in hospital especially those with frailty, cognitive impairment and decreased mobility. It is anticipated that through improved focus on minimising harm there will be overtime a reduction in hospital acquired complications such as falls, pressure injury, delirium, malnutrition and infection (urinary tract infection and pneumonia).
Comprehensive Care – Minimising Harm model
To undertake an improvement project, there must be an issue or problem that you aim to improve, for example:
- High falls rate on ward
- High number of patients developing delirium or with confusion
- High rate of pressure injuries
- No early and safe mobilisation for patients
- Safety Huddles aren't being completed on our ward
- Intentional Rounding isn't being completed reliably
- Identification, management and communication of patient risk factors are not occurring reliably
At this stage of the project, it is about identifying the problem you aim to improve NOT brainstorming solutions.
When determining the focus of an improvement project, some common errors include:
- Selecting a problem no one is interested in
- Implementing a solution rather than investigating a problem
- Focusing on a process that is currently in transition or unstable, for example, manual to electronic process
- Selecting a problem that is beyond your capability to change or outside your sphere of influence.
Once you have identified the problem, add this to the project:
| |
All improvement requires change. However, change is not always welcomed or accepted by individuals or teams, even when it is improvement focused. Improvement projects can often struggle to gain momentum if there is considerable resistance from those who will be impacted most by changes.
Assessment of the current unit/ward context is essential to clearly establish the readiness for change. The assessment should investigate the existing culture, communication and team practices, and safety and quality concerns. If there is an overall lack of enthusiasm and a resistance to change, it is vital this is addressed before proceeding further with the improvement project. For more information see the CEC Safety Culture webpage.
Data will assist in identifying the problem and build the evidence base about why this is an important problem to focus on. Seek guidance from your Clinical Governance Unit or the CEC to identify appropriate sampling numbers and data sources.
Existing data: Examine your health service’s data via incident data from your incident management system (ims+), QIDS Data, review of any RCA incident reports, local audit data and other sources.
Baseline audit Completing a baseline audit is also an effective way to identify the problem. The Comprehensive Care – Minimising Harm Baseline audit tool can be used it is an effective way to identify the problem.
Staff and patient stories: gaining information about the experience of the change can provide different insights into program processes, show impact, identify unintended consequences, demonstrate innovation and support the quantitative data.
Literature search: Further information can be gathered by searching the literature.
| The Comprehensive Care – Minimising Harm Baseline Data Collection template can be found via the | |
The improvement project brief is essentially a document that outlines your improvement project. It should include what the problem is, why is it important (to patients, their families, staff and the broader community), how long it will take to do and the approach you will use to achieve an improvement.
A strong improvement project brief should be founded on the supporting data you have collected, should take into consideration how the improvement will be sustained and align with your health service's priorities. You can use the improvement project brief to help with gaining support for your improvement project.
| The Comprehensive Care improvement project brief - template can be found via the | |
It is strongly recommended that you engage with your Clinical Governance Unit to seek support for and during your improvement project. Your Clinical Governance Unit will be able to link you with local quality improvement experts.
You may also choose to reach out to colleagues in other health services to find out how they approached their improvement work, including their successes and learnings.
How do you gain leadership support for your improvement project?
It is essential to gain leadership support from within your health service as all improvement projects require an investment of time, resources and commitment at every stage of the project.
Use your Improvement Project Brief to gain a project sponsor. The project sponsor is someone who can provide support and guidance to you during the improvement project. They can help with ensuring appropriate resources are provided and help remove barriers when needed. Ideally, your project sponsor is someone who does not work directly on the improvement project but is in a senior position.
The level of seniority of the project sponsor will depend on the scope of your improvement project (for example, Nurse Unit Manager versus an Executive Director). Ideally you should communicate closely with the project sponsor and provide regular updates.
Your project sponsor will be able to provide guidance on where the governance for your improvement project will sit within your health service. This will ensure there is operational responsibility for the improvement project and a channel to report back on how the improvement project is progressing. For example:
- At unit/ward level: Integrate project reporting with existing ward staff meetings, display ward data e.g. xx days since last fall
- At Facility: Reporting can be integrated with the existing Health Care Quality Committee's
- At health service/LHD/SHN level: Integrate project reporting with oversite through existing Comprehensive Care Committee.
Note this is different from your project team structure. Your project team will consist of members who carry out the project interventions.
Who should be in your improvement project team?
The improvement project team should be interdisciplinary and include the right people, with the right experiences, expertise, and interest in contributing. For example:
- Team leader
- Quality improvement advisor/expert
- People from all areas of the process the improvement project will target, including junior and senior staff
- Consumer representative (or interview / survey consumers)
- Consider inviting colleagues who are likely to challenge your project. They can often raise different perspectives or barriers that you may not have considered.
The team leader role is essential, and they will organise and lead the team meetings, ensure delegation of responsibilities and be the 'voice' for the improvement project.
An example team may include:
- Team Leader
- Medical staff – junior and senior
- Nurse Unit Manager or Clinical NUM/Navigator
- Clinical Nurse Consultant and/or Clinical Educator
- Nursing staff who work on the ward
- Physiotherapist
- Dietician
- Occupational Therapist
- Pharmacist
- Quality Advisor
- Consumer/s/families
Once the project team is formed, add each member to the project.
| |
As the team leader, it is essential to assemble a dedicated team who are also committed to actively supporting the improvement project. Improvement projects often fall down when team members are unable to sustain interest or participation in the improvement project, leaving the team leader to carry the improvement project.
The role of the project team includes:
- Evaluating current processes
- Identifying and enlisting clinical champions
- Establishing general goals
- Developing, implementing and evaluating improvement strategies
- Disseminating results and findings.
Once the project team has been established, it is important to make sure everyone is on the same page regarding the problem the improvement project is targeting and what is IN and OUT of SCOPE. Without a well-defined scope, improvement projects tend to grow beyond what is achievable, lose focus of the problem and fail.